While much has been made of support expressed for the introduction of the National Health Insurance, a closer assessment of presentations on the NHI Bill during parliamentary hearings suggests that a number of concerns still need to be addressed.
Support for aim but not strategy?
We carried out an analysis of 75 submissions heard between 18 May and 8 December 2021. The findings suggest:
- That many respondents support the goal of achieving Universal Health Care (UHC) but not the NHI as it is outlined in the Bill; and
- That while there is broad support for the aims of the Bill (attaining UHC), many have doubts as to whether the strategy as set out in the Bill will deliver UHC.
We found three groups of respondents that could be defined by levels of support for the Bill.
The first group consisted of those who have unequivocally come out in support of NHI. For example, the National Health Laboratory Service (NHLS) stated that it is “fully supportive of the introduction of the NHI Bill”; and the South African Nursing Council indicated that it “welcomes the NHI, an initiative to improve access to quality health services in the Republic of South Africa”.
The second group consists of those who were unequivocally against the Bill. The De Klerk Foundation, for instance, submitted that “the proposed NHI Bill does not provide the answer to achieve UHC”. Oticon were of the view that “…having one funder can cripple the health industry of the country and create barriers to access, the very barriers that the NHI is attempting to breach… We, therefore, propose there be a multiple funder system”. And the Free Market Foundation pointed out that “only one developing economy (Cuba) has ever built an equivalent to NHI (i.e. a monopoly single-payer system)… So why is the NHI being pursued if we know Cuba’s total health spend = 13% of GDP … Why are warnings by Treasury and Davis Tax Committee on the lack of affordability of NHI being ignored?”
The third group consisted of respondents whose support for the Bill was ambivalent, with most of them declaring support for UHC or the aims of the NHI, but conditional or unclear support for the NHI per se. For instance, the National Planning Commission (NPC) stated that it “supports the key policy principles essential for universal health coverage reform, [that is] mandatory contribution, pooling of funds and strategic purchasing to promote efficiency and accountability”. However, it cautioned that “the NPC sees the Bill as a step in the right direction, but it submits that the Bill in its current form is lacking in critical detail in some important areas and contains provisions that are problematic.” The Board of Healthcare Funders (BHF) indicated in its submission that while it supports the concept of Universal Health Care, “it is necessary to emphasise National Health Insurance is not UHC. NHI is just one of the mechanisms for achieving the objectives of UHC … BHF also supports the concept of NHI and has done so since 2008. However, in order for it to work effectively, there are certain criteria that must be satisfied.” The Khayelitsha and Klipfontein Health Forums stated that “In principle, there is support for the purpose of the NHI Bill that seeks to achieve universal access to quality health care services in the Republic in accordance with section 27 of the constitution. However, the success of the NHI Bill is dependent on a strong Public Healthcare System and the challenges experienced by the Public Healthcare System need to be addressed and fixed as a matter of priority. Failing this, we will be setting up the NHI to fail”.
To assess the overall level of support and the nuances in the level of support we compared the level of support for UHC and the level of support for NHI.
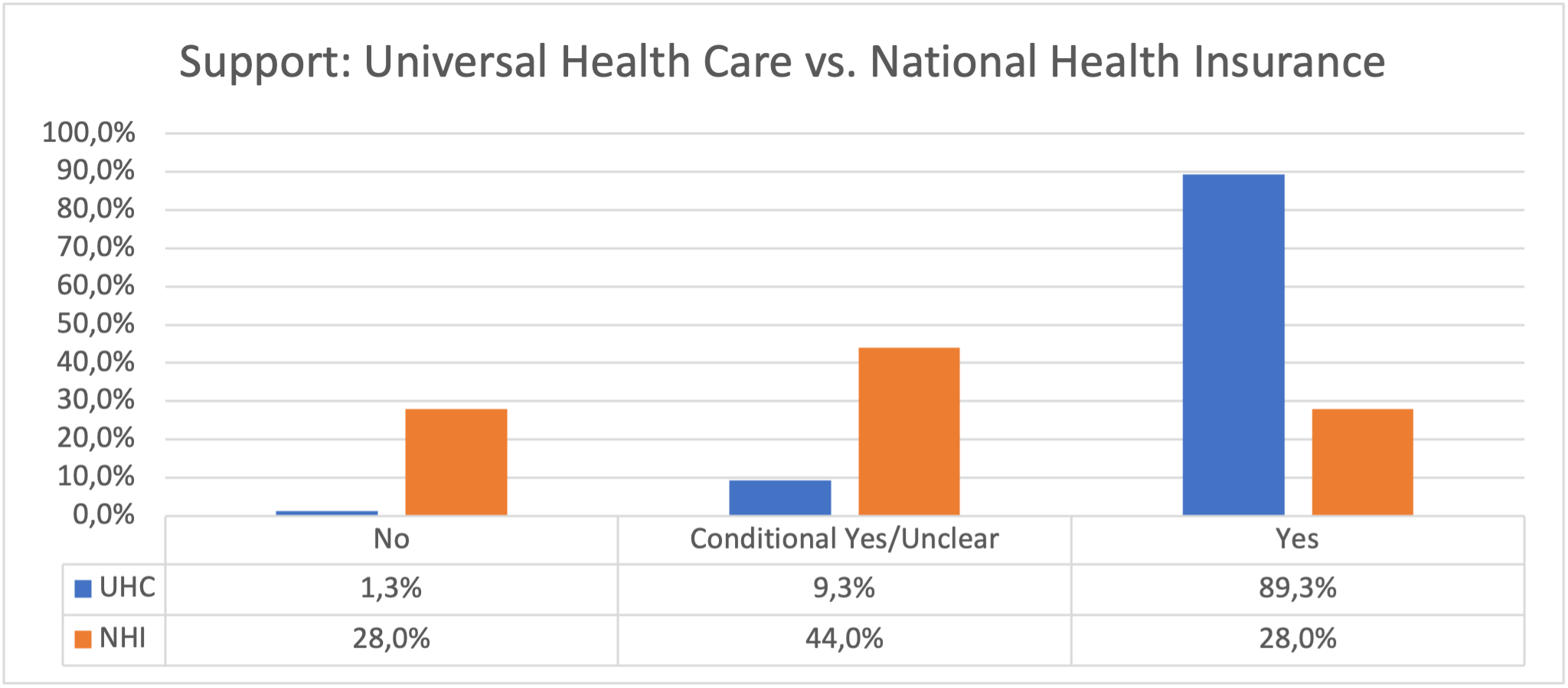
There was a significant difference between the levels of support for UHC and NHI, with 89.3% of respondents supporting UHC, just 1.3% against and 9.3% conditional/unclear. For NHI, 28% were in support, 28% were against and 44% were conditional/unclear.
The findings suggest that while there is broad support for the aims of the Bill (attaining Universal Health Care), many have doubts as to whether the strategy as set out in the Bill will deliver this; support for the NHI per se is much lower. This is not surprising: it is easier to support an aspirational goal (especially one that has been left open to interpretation as neither the Bill nor respondents clearly define UHC) than it is to agree on a strategy to achieve that goal.
By seeking to “establish and maintain a National Health Insurance Fund in the Republic funded through mandatory prepayment that aims to achieve sustainable and affordable universal access to quality health care services” the Bill sets out a very particular strategy to address various flaws and challenges in the current organisation and structure of the health system in South Africa and to move towards UHC. However, respondents have a range of concerns around the proposed strategy.
Concerns regarding the ability of NHI to deliver UHC
We also examined the responses to better understand the main concerns regarding the Bill among those who were either opposed to it or conditional/unclear in their support.
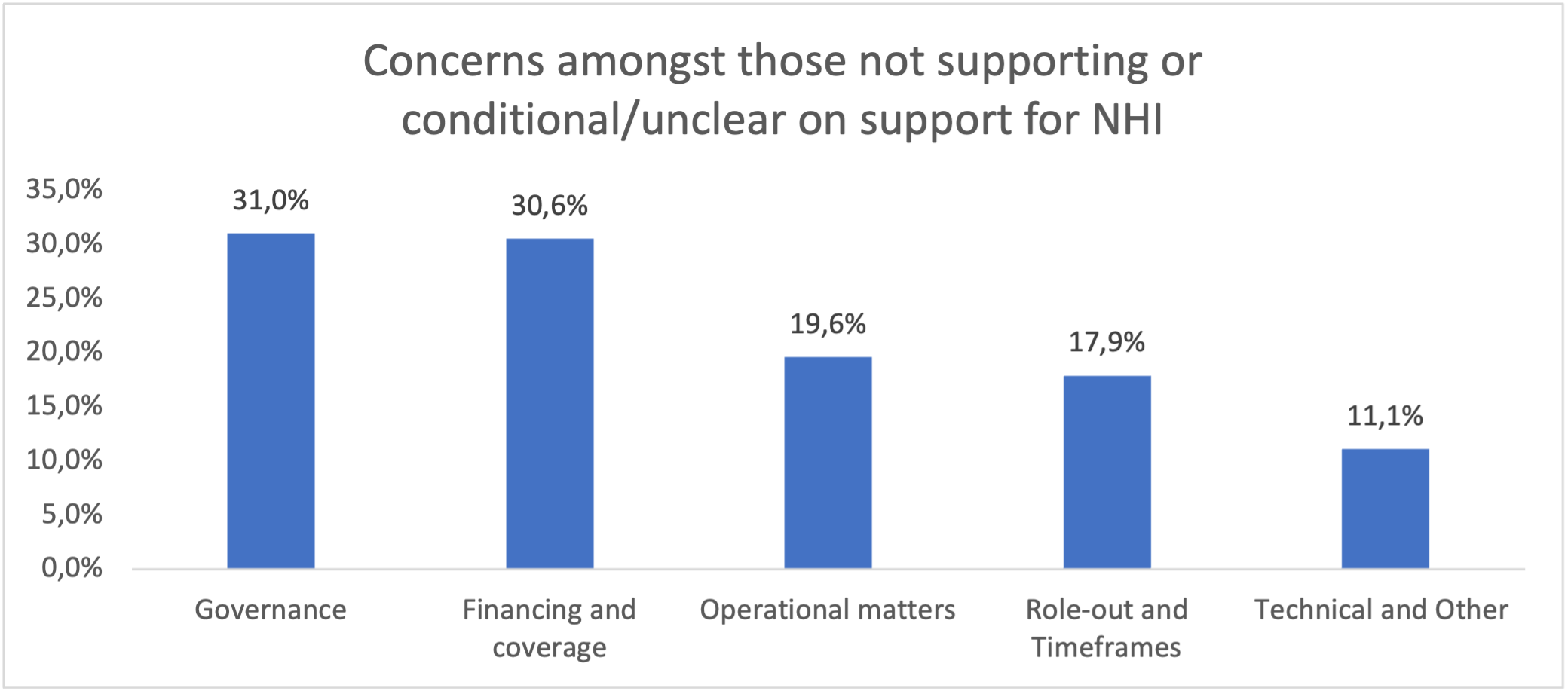
Concerns around governance, leadership, management, corruption and capacity and the impact of these factors on the ability of the NHI reforms to deliver UHC featured most prominently at the hearings. This was followed by concerns related to the lack of clarity on the financing of NHI and/or the availability of funding for the NHI, and coverage and range of benefits. Many respondents raised concerns around a range of operational issues such as the data and information systems, accreditation process, appeals processes, procurement and the health technology assessment capability that would be required to support NHI. The rollout of NHI, transitional arrangements and timeframes for implementation and the poor state of public sector facilities were also common concerns. The last group of concerns related to some of the technical aspects of the Bill including definitions, general editing/language in the Bill, legislation to be repealed and the explanatory memorandum.
Portfolio Committee response?
The portfolio committee could pass the Bill without any changes or with only minor amendments; it could make substantive amendments to the Bill to address the concerns raised, or it could reject the Bill. Notwithstanding the potential for bias against the Bill amongst the respondents choosing to present to the hearings and the incomplete sample on which we analysed the responses, the low level of “unequivocal” support for the Bill together with the broad range of concerns expressed suggests that it would be prudent for the portfolio committee to meaningfully address these concerns. This would ensure broader public support for the Bill, even if this means a further delay in passing it. National Health Insurance is one of the largest reforms proposed since 1994 and the approach taken by the portfolio committee will have a profound impact not only on the future health system but also on the broader trajectory of social, societal and economic well-being in South Africa. DM
By Geetesh Solanki, Stephanie Wild, Judith Cornell and Vishal Brijlal
Geetesh Solanki is Specialist Scientist at the Health Systems Research Unit, SA Medical Research Council (SAMRC); an Honorary Research Associate in the Health Economics Unit, University of Cape Town and Principal Consultant at NMG Consultants and Actuaries; Stephanie Wild is a post-graduate student enrolled for a MPhil in Public Law at the University of Cape Town; Judith Cornell was the Director of Institutional Development and Planning (now retired) at the Nelson Mandela School of Public Governance, University of Cape Town, South Africa; Vishal Brijlal is a Senior Director at the Clinton Health Access Initiative. The opinions expressed are those of the authors and do not necessarily reflect the views of their institutions.
Original Article available on the Daily Maverick Website

