There has been a significant rise in new SARS-CoV-2 infections in the Gauteng Province in the last four weeks which has been attributed to the new Omicron variant announced on 24 November 2021. The first cases of Omicron were detected in the Tshwane District and coincided with the sharp rise in new infections, heralding the onset of the fourth wave in Gauteng.
Tshwane has been the global epicentre of the Omicron Outbreak and the Gauteng Province Fourth Wave with the weekly number of cases rising exponentially over several weeks, reaching just over 8569 cases in Epi Week 47 (21 November - November 27 and 41 921 by 3 December before the end of Epi Week 48 (28 November to 4 December). The exponential rise in cases has continued with 9929 new cases reported in Tshwane in the last 5 days from 29 November to 3 December 2021 (Figure 1).
We report on the early experience of the patient profile at the Steve Biko/Tshwane District Hospital Complex in Pretoria, in the heart of the Tshwane District.
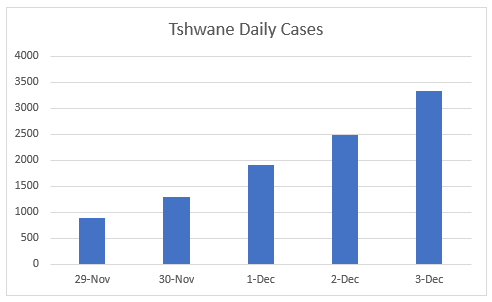
Fig 1. Daily New SARS-CoV-2 Cases 29 November – 3 December 2021 (sacronavirus.co.za)
In keeping with the statistics presented by the Gauteng Department of Health on 2 December 2021 for the province as a whole, and with admissions across all public and private hospitals in Tshwane as shown in the NICD DATCOV database, we have seen a sharp rise in admissions at the Steve Biko Academic and Tshwane District Hospitals (SBAH/TDH) Complex with 166 new admissions between 14 and 29 November 2021. This makes up 45% of all Tshwane District Admissions in the public sector and 26% of all admissions in both public and private sectors for the same period.
It is essential to recognize that the patient information presented here only represents the first two weeks of the Omicron wave in Tshwane. The clinical profile of admitted patients could change significantly over the next two weeks, by which time we can draw conclusions about the severity of disease with greater precision.
Though the NICD has confirmed that almost all cases of SARS-C0V-2 in Tshwane are due to the new variant, we have not been able to establish that in every instance the variant is Omicron as the PCR machine in use at the SBAH laboratory does not screen for the S-gene. A reasonable assumption is being made that the cases described here represent infection with the new variant.
|
||||||||||||||||||||||||||||||
This is a picture that has not been seen in previous waves. In the beginning of all three previous waves and throughout the course of these waves, there has always only been a sprinkling of patients on room air in the COVID ward and these patients have usually been in the recovery phase waiting for the resolution of a co-morbidity prior to discharge. The COVID ward was recognizable by the majority of patients being on some form of oxygen supplementation with the incessant sound of high flow nasal oxygen machines, or beeping ventilator alarms.
There are only 4 patients in high care and one in the ICU. The numbers of patients in high care on double oxygen, High Flow Nasal Oxygen or non-invasive ventilation (NIV) were noticeably higher in previous waves. This is anecdotal but confirmed by numerous clinicians who have previously worked in the COVID wards in the hospital complex.
|
||||||||||||||||||||||||||||||||||||
A key question regarding the new Omicron outbreak is whether disease severity is similar, milder or more severe than with the other variants, given the large number of Omicron mutations.
The best indicator of disease severity is measured by the in-hospital death rate. There were 10 deaths in the SBAH/TDH cohort in the past two weeks, making up 6.6% of the 166 admissions. Four deaths were in adults aged 26 – 36 and five (5) deaths were in adults over 60. One death was in a child in whom the cause of deaths was unrelated to COVID. There were no COVID related deaths among 34 admissions in the paediatric COVID wards over the last two weeks. This compares favorably to the proportion of deaths at the complex over the past 18 months which was 17%. The trend over the next two weeks will be clarified as the number of deaths is currently low, and sufficient time will have elapsed for the development of greater severity of disease and the number of deaths might be expected to increase. For now, the death rates over the last two weeks.as well as over the past 18 months at the SBAH/TDH complex are lower than the overall in-hospital death rate of 23% for the country over all previous waves, as reported by the NICD.
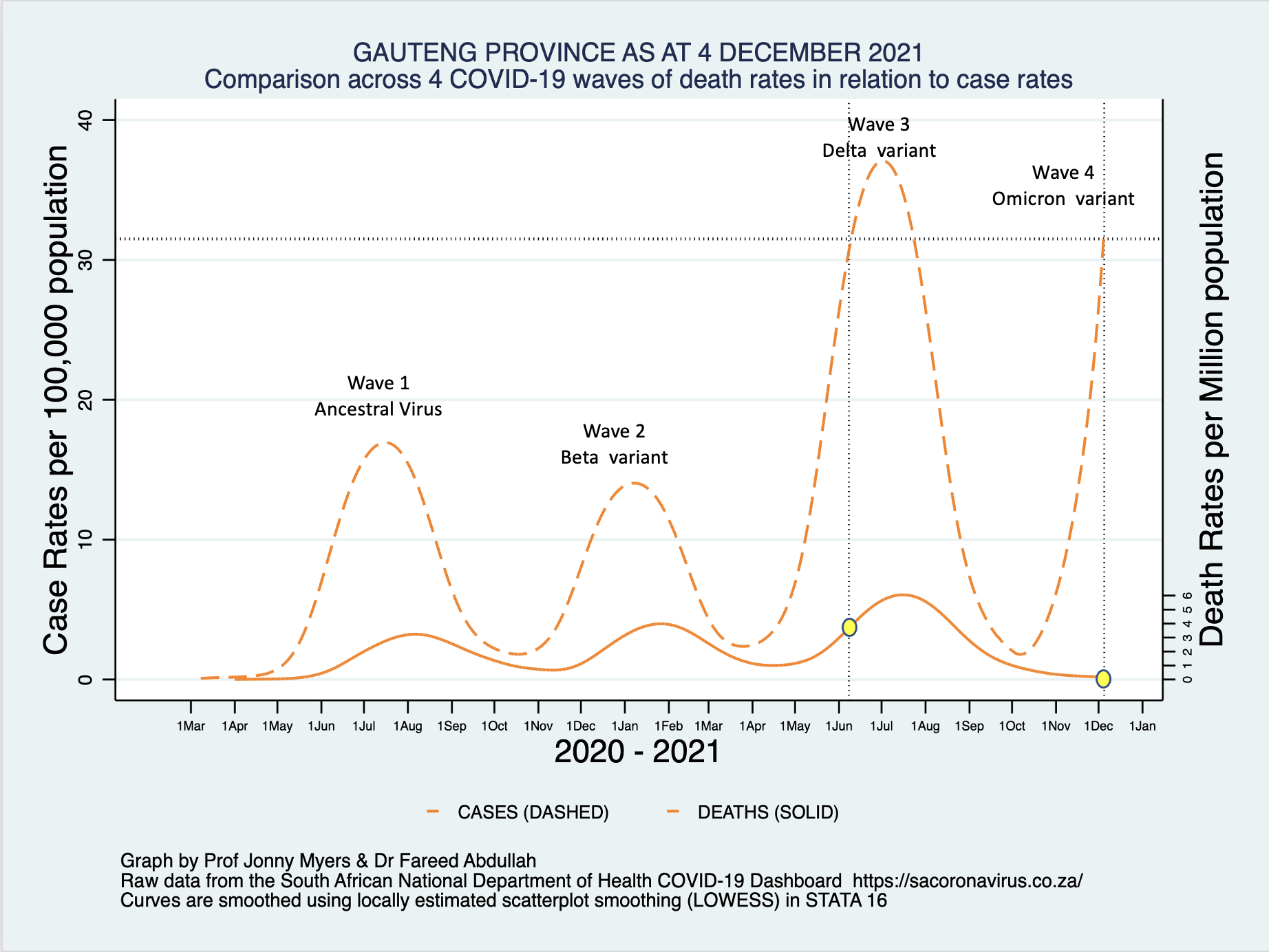
Figure 2 below shows the absence of any significant increase in in-hospitals deaths in relation to the dramatic rise in the case rate for the Gauteng Province as a whole. This may be due to the usual lag between cases and deaths and the trend will become clearer over the next few weeks.
Figure 2. NEW SARS-CoV-2 Case and COVID-19 Death Rates Gauteng Province (graph courtesy of Professor Jonny Myers, UCT) (solid red line indicates date of commencement of vaccination rollout)
Other crude indicators of severity of disease include the level of care required in hospital (ICU, high care, general ward), oxygen requirements (nasal prongs, face mask, high flow, non-invasive or invasive ventilation) and length of stay in hospital.
Figure 1. Level of Care of Patients Over Last Two Weeks
There were only 2 patients in the COVID ICU in the last 14 days, neither of whom had a primary diagnosis of COVID pneumonia. Sixty-three patients were admitted to high care, but our anecdotal information is that the majority of high care admissions were for a diagnosis other than COVID.
In the snapshot Table 1 above, 3 of the 4 patients in the high care ward had a primary diagnosis of severe COVID pneumonia so it could be that the more recent profile is changing to more severe COVID disease. A more detailed analysis of high care patients is being conducted and may be more revealing.
More precise measures of severity of disease in hospitalized individuals require a review of Chest X-Ray or lung Computer Tomography findings (percent of lung fields showing changes), blood gas measures, blood biomarkers and the concomitant effect of co-morbidities on the patient’s condition. Detailed studies of both the crude and more precise measures of disease severity are being done locally by several teams of researchers and the team at Steve Biko is participating in these studies.
A significant early finding in this analysis is the much shorter average length of stay of 2.8 days for SARS-CoV-2 positive patients admitted to the COVID wards over the last two weeks compared to an average length of stay of 8.5 days for the past 18 months. The NICD reports a similar shorter length of stay for all hospitals in Tshwane in its weekly report. It is also less than the Gauteng or National average length of stay reported by the NICD in previous waves.
In summary, the first impression on examination of the 166 patients admitted since the Omicron variant made an appearance, together with the snapshot of the clinical profile of 42 patients currently in the COVID wards at the SBAH/TDH complex, is that the majority of hospital admissions are for diagnoses unrelated to COVID-19. The SARS-CoV-2 positivity is an incidental finding in these patients and is largely driven by hospital policy requiring testing of all patients requiring admission to the hospital.
Using the proportion of patients on room air as a marker for incidental COVID admission as opposed to severe COVID (pneumonia), 66% of patients at the SBAH/TDH complex are incidental COVID admissions. This very unusual picture is also occurring at other hospitals in Gauteng. On 3 December Helen Joseph Hospital had 37 patients in the COVID wards of whom 31 were on room air (83%); and the Dr George Mukhari Academic Hospital had 80 patients of which 14 were on supplemental oxygen and 1 on a ventilator (81% on room air).
The exponential increase in the positivity rate in these patients is a reflection of the rapidly increased case rate for Tshwane but does not appear to be associated with a concomitant increase in the rate of admissions for severe COVID (pneumonia) based on the high proportion of patients not requiring supplemental oxygen.
The relatively low number of COVID-19 pneumonia hospitalizations in the general, high care and ICU wards constitutes a very different picture compared to the beginning of previous waves. A detailed analysis comparing the current picture with previous waves is still being conducted. This may very well be related to the early upswing of the fourth wave, with the more classical pattern becoming evident over the next two weeks. What is clear though is that the age profile is different from previous waves. It may be that this is a vaccination effect as 57 % of people over the age of 50 have been vaccinated in the province compared to 34% in the 18-to-49-year group.
The high proportion of COVID incidental adult patients and the increased number of SARS-CoV-2 positive admissions among children aged 0-9 may reflect higher rates of community transmission compared to previous waves (variants) that is not translating into higher admission rates for a primary COVID-19 diagnosis. More time is required to fully answer the questions about the severity of COVID-19 caused by the new Omicron Variant.
View more - Tshwane District Omicron Variant Patient Profile - Figures and Tables
Updated Report available on the International Journal of Infectious Diseases Website - 28 December 2021
Author: Dr Fareed Abdullah
Dr Fareed Abdullah is the Director of the Office of AIDS and TB Research at the SAMRC and a part time HIV Clinician at the Steve Biko Academic Hospital. Since the beginning of the COVID-19 pandemic he has worked as a member of the COVID-19 clinical team through the first three waves of the epidemic.
Acknowledgements
- Professor Jonny Myers, UCT
- Professor Glenda Gray, President and CEO, SAMRC
- Professor Veronica Ueckermann and senior clinicians from the Steve Biko Department of Internal Medicine
- Professor Deb Basu and colleagues from the Department of Public Health, University of Pretoria
- Dr Raj Ramlall and clinicians from the Tswhane District Hospital
- Dr Lucille Blumberg, NICD and Right to Care
- Dr Waasila Jassat and Dr Richard Welch, NICD
More information: