Improving diabetes diagnosis in African populations
 Cape Town | Results of a South African study conducted by a group of investigators from the South African Medical Research Council (SAMRC), Cape Peninsula University of Technology (CPUT), Stellenbosch University (SU) and the US National Institute of Health (NIH) have demonstrated for the first time in an African population, the added value of combining glycated haemoglobin (HbA1c) and glycated albumin (GA) to diagnose dysglycemia, the combination diabetes mellitus and pre-diabetes.
Cape Town | Results of a South African study conducted by a group of investigators from the South African Medical Research Council (SAMRC), Cape Peninsula University of Technology (CPUT), Stellenbosch University (SU) and the US National Institute of Health (NIH) have demonstrated for the first time in an African population, the added value of combining glycated haemoglobin (HbA1c) and glycated albumin (GA) to diagnose dysglycemia, the combination diabetes mellitus and pre-diabetes.
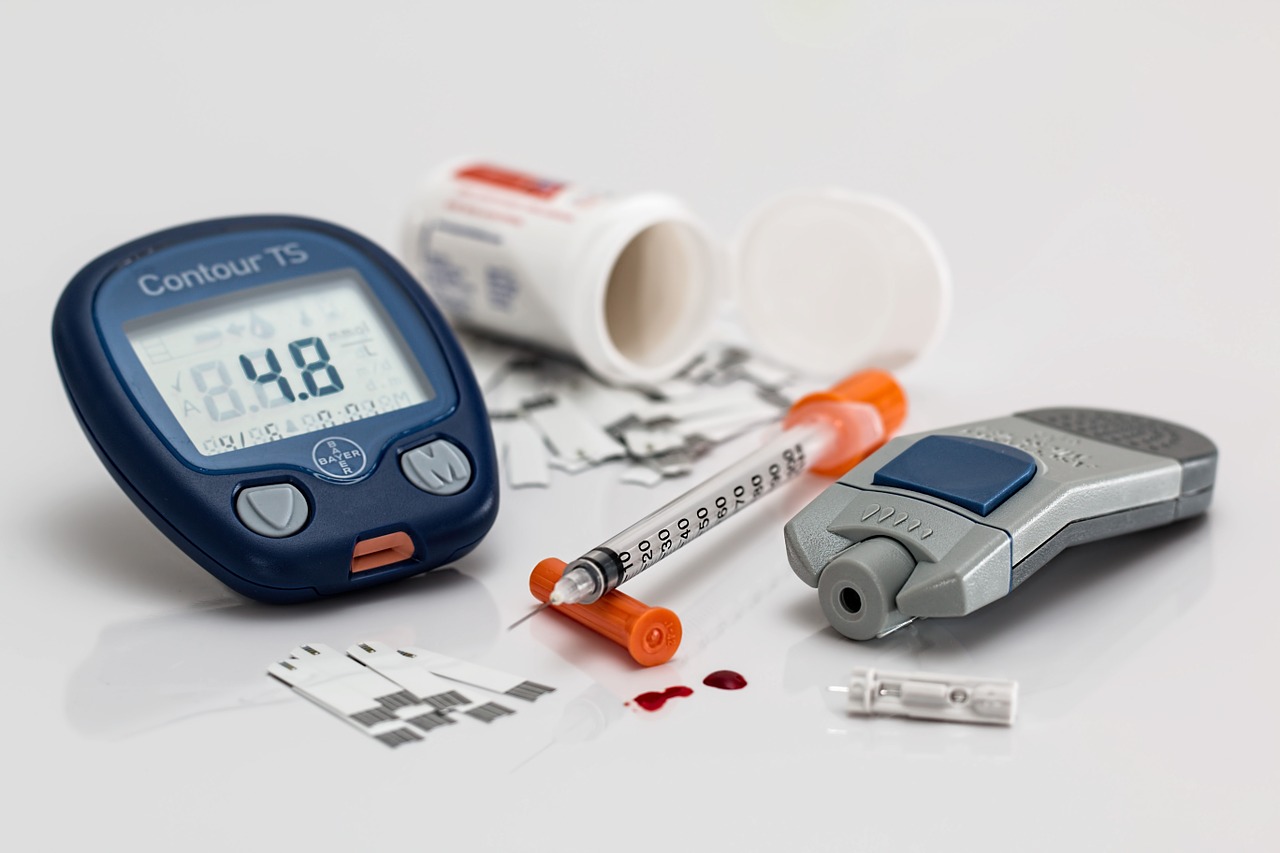
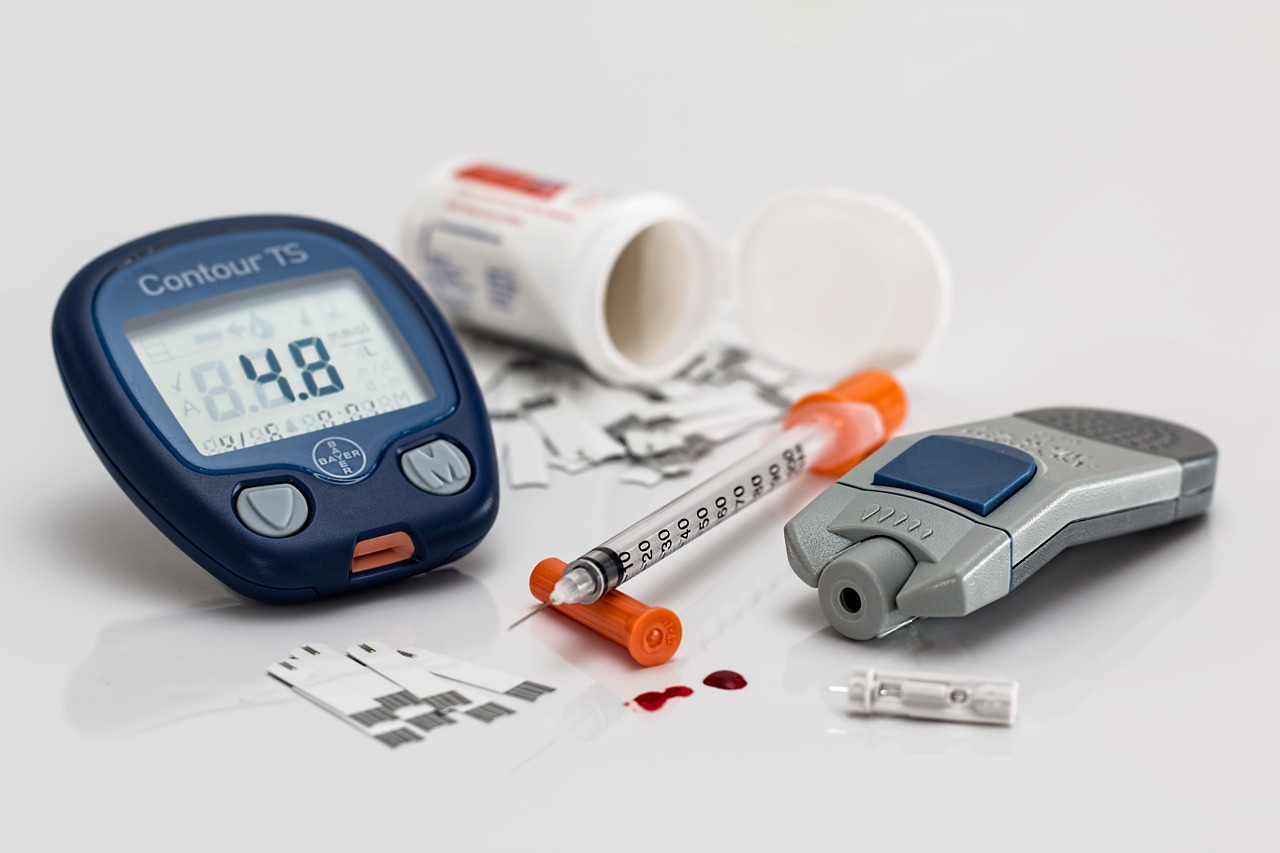
Diabetes mellitus, which is a condition characterised by chronic elevation of blood sugar, is a fast-growing disease worldwide, and much so in countries in sub-Saharan Africa (SSA) where the number of people with diabetes is estimated to increase by 134% from 24 million in 2021 to 55 million by 2045, according to the International Diabetes Federation (IDF). South Africa (4.2 millions), Nigeria (3.6 millions), Tanzania (2.9 millions), Ethiopia (1.9 millions), and Democratic Republic of Congo (1.9 millions) are currently the top five SSA countries for the number of people with diabetes. Diabetes in SSA is further characterised by the low detection rates, with about 54% of SSA people with diabetes being unaware of their condition; against 44.7% at the global level.
The low diabetes detection rate in Africa is explained by a number of factors including the lack of screening programs, the low prioritisation of large segments of the population (young adults and non-obese people) for diabetes screening where programs are available, and the lack of accurate and practical diagnostic approaches.
In this first detailed study in an African population, the investigators used data for nearly 1300 adults mixed-ancestry South African residing in Cape Town to examine the ability of glycated haemoglobin (HbA1c) and glycated albumin (GA) in combination to diagnose diabetes or dysglycemia. HbA1c and GA are both tests used to monitor blood sugar control in response to treatment in people with diabetes; but, have also been proposed for diabetes diagnosis, although not yet widely adopted in the African settings due to their variable performance. “In mixed-ancestry South African, HbA1c and GA levels varied in opposite directions with increasing levels of adiposity as measured by the body mass index (BMI). As a consequence, combining the two tests improved the detection of dysglycemia above and beyond the achievements of each test taken separately, and this improvement was observed across all levels of BMI” says Professor Andre Pascal Kengne, the lead author of the publication, and Director of the Non-Communicable Diseases Research Unit (NCDRU) at the SAMRC.
Unlike other diagnostic tests for diabetes, HbA1c and GA do not require fasting. “These findings in mixed-ancestry South Africans are in line with results from our previous studies in African-born Blacks living in America, which have shown that combining HbA1c and GA improves dysglycemia diagnosis, particularly in individuals who are non-obese,” says Dr. Anne E. Sumner, senior author on the paper and Senior Investigator in the Section on Ethnicity and Health, Diabetes, Endocrinology, and Obesity Branch, National Institute of Diabetes and Digestive and Kidney Diseases, part of the National Institutes of Health in Bethesda, Maryland, USA. “This study suggests an approach that can be operationalised and incorporated into existing screening programs for diabetes in African settings,” adds Dr. Sumner.
Data used for the current study are from the Cape Town Vascular and Metabolic Health (VMH) project, which is an extension of the Bellville South research program initiated in Cape Town in 2008. “These new findings are a very useful addition to our efforts to improve the understanding, prevention, detection and control of common cardiometabolic diseases in mixed-ancestry South Africans and other African populations over the last two decades” says Prof Tandi E Matsha, co-lead author of the paper, Principal investigator of the VMH project, Dean of the Faculty of Health and Wellness at CPUT, and Director of SAMRC/CPUT Extra-mural Cardiometabolic Health Research unit.
“Population-based screening for common chronic infectious diseases such as HIV infection is already taking place across Africa using minimally invasive blood sample collection” note the investigators. “Adding HbA1c and GA to these programs provides an opportunity to co-screen people for dysglycemia’ they conclude. HbA1c is already available as point-of-care test and similar approach can be developed for GA.
NOTE TO THE EDITOR:
The study was published in eClinicalMedicine, a Journal of The Lancet group with the title “Combining HbA1c and glycated albumin improves detection of dysglycemia in mix-ancestry South Africans”; and is fully accessible here: https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(22)00173-0/fulltext.
The VMH project was funded by the South African Medical Research Council.
Contact Details
Tendani Tsedu
Head of Corporate & Marketing Communication
Email: tendani.tsedu@mrc.ac.za